Effective Nurse Communication With Type 2 Diabetes Patients a Review
Practice nurses are at the forefront of intendance for people with type 2 diabetes. Patients require high-quality guidance and back up on how to cocky-manage their condition (Department of Health, 2001). Practice nursing is a highly democratic role, and it is therefore imperative that nurses have the essential skills and noesis to back up their patients. Although role-based factors shape practice, nurses' dispositional qualities are also likely to influence the mode in which they support people with such a complex status (Ingulli et al, 2014). Enhanced insights into how practice nurses assist people with type 2 diabetes tin can inform service providers on how to deliver meliorate back up to people with this status.
Groundwork
Type 2 diabetes is an ever-growing national and international concern but, despite this, the bear upon of the disease continues to grow (Hicks, 2015; Valabhji, 2018). As well as its physical effects, type 2 diabetes has a substantial emotional impact upon people with the condition and their families (Berry et al, 2019). In addition, type two diabetes has substantial socioeconomic implications; its treatment accounts for just under 9% of the annual NHS budget, around £viii.8 billion per annum (Diabetes UK, 2018). It is therefore essential that effective support for people with blazon 2 diabetes is achieved.
Report aim
The aim of the electric current research was to evaluate how nurses in a master care setting back up the self-management of people living with type ii diabetes.
Methods
This commodity conveys the cardinal findings from research that investigated the perspectives of practice nurses who are directly involved in the care of people with type 2 diabetes. The research was conducted within the W Midlands region of the UK. Ethical clearance for the report was obtained from Staffordshire Academy and the NHS Health Research Say-so (HRA).
A qualitative research strategy was employed, which included semi-structured interviews. All participants were required to be working as a practice nurse, supporting people with type 2 diabetes, and to have a minimum of one yr's experience in this role. Invitation letters and information sheets were sent via do managers to potential participants. These communications highlighted that participation was voluntary and that participants could withdraw at whatsoever point of the study without needing to offering an explanation.
In the interviews, respondents were invited to talk over their feel of, and perspectives on, the support of people with type ii diabetes in chief care settings. This enabled in-depth insights into nurses' perspectives to be obtained. A semi-structured interview method was adopted, which followed a flexible approach with open-concluded questions. While a topic guide shaped the interviews, this flexibility ensured interviewees were complimentary to raise matters that were important to them. The topics covered included the experience of participants in supporting people with type 2 diabetes; how participants assisted patients to achieve self-efficacy; available resources to support the practice nurse office; and perspectives on how the practise nurse role can facilitate good intendance. Participants were interviewed until information saturation was achieved. The interviews had a hateful elapsing of approximately 30 minutes.
A process of thematic analysis was undertaken to analyse the responses. This required reading and re-reading of transcripts, closed-coding of the text and the organisation of these codes into broader themes (Braun and Clarke, 2006). This procedure enabled the key content of interviews to be established and addressed commonalities (and difference) across participants' accounts. The three principal themes identified were skills and dispositional qualities; accessing resources; and medication and prescribing.
Results and give-and-take
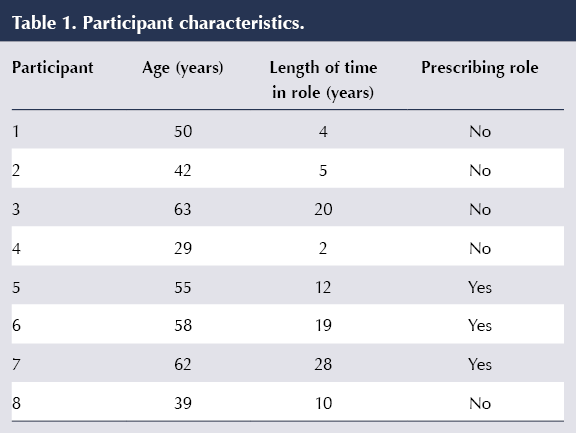
Eight practice nurses participated in the study. Although there was no exclusion criterion on gender, the sample consisted of female nurses only. Participant characteristics are shown in Table 1.
The themes that emerged from the interviews are discussed below.
Theme 1: Skills and dispositional qualities
All participants acknowledged multiple skills and qualities that they felt enhance the cocky-management and motivation of people living with type two diabetes. A commonality across the interviews was recognition of the importance of building a skillful rapport with patients and the centrality of good communication skills in achieving this rapport. 1 of the biggest barriers healthcare professionals run across is meeting and understanding the needs and continued demands of people with type 2 diabetes (Shrivastava et al, 2013). Participant 1 best-selling the centrality of communication to good do when discussing how the nurse–patient relationship could be successfully supported:
"…definitely down to advice yeah, you've got to be on their level, yous've not got to be this strict tyrant who's going to be, y'all know, preaching at them. I think that merely starts with the walls coming upwards."Participant 1
Empathy and understanding are also required for ensuring that communication meets person-centred requirements. Delivering individualised communication, tailored to patient demand, is considered paramount. This is crucial when the care is of a facilitative nature:
"I try and discover what they enjoy and what their motivating triggers and barriers are; in that location's no point telling someone to go out running one nighttime a week if they don't enjoy information technology considering they won't exercise it. Or to nourish a slimming class if they are skint or lack in confidence, considering they merely won't go." Participant 8
This quote also shows how an agreement of patients' needs has to exist reconciled with realistic goal setting and clear planning (Polonsky et al, 2010). Empathy and understanding are key qualities but these demand to exist complemented past clear, effective approaches to setting goals and management planning. Information technology is worth noting, nevertheless, that this differs from the imposition of external targets, which could exist an impediment to person-centred back up as, if an excessive emphasis is placed on the importance of targets, information technology could divert attention from aspects of care that are less acquiescent to measurement (Harwood et al, 2013).
Communication needs to be purposeful and grounded in the nurse's self-directed planning and arrangement. This is addressed further in the following quote, in which it is highlighted how documentation skills are vital as a fashion of ensuring that letters could be revised according to patient responses:
"…I always document carefully and I could see I had seen him for the past three years and he had washed nothing different at all and I was just saying the same things, so I said to him can I just ask what you get out of coming here because for the last three years I've told yous the same things and you've washed nothing almost information technology, and he said to me he did not sympathise how to change his diet." Participant 3
Theme 2: Accessing resources
The wider availability of resources provided to heighten patients' self-management of type 2 diabetes was discussed by all participants. Information technology was highlighted that there was limited access to any healthy lifestyle services (Peter et al, 2011), as previous services had been decommissioned and, consequently, the majority of lifestyle management was now undertaken in-house by the practice nurses:
"Nosotros used to have lots of services… most of that stuff has been taken abroad from usa; it's a difficult ane really, it'southward like your smoking cessation has been taken away from us. I mean what'southward the all-time affair to tell a diabetic to exercise: stop smoking, isn't it really, to cease them getting peripheral arterial affliction, merely there's nowhere to send them." Participant 6
Diabetes is often linked with depression; this might increase pessimistic feelings, and a lack of self-efficacy could potentially demotivate individuals from making the changes required to self-manage their status (Graffigna et al, 2014; Nash, 2015). Participant 8 considered dealing with these underlying problems to be a priority in the improvement of self-management:
"I call up it is important to deal with any underlying issues that can stop patients managing their diabetes. Depression is a biggie; I effort and tackle this with patients and become them to engage with the wellbeing services before I knock them further putting more pressure on them. I call back the better a patient is in their mind, the easier it is to get them to engage." Participant eight
Practise nurses are at the forefront of care, even so their limited time with patients can be spent finding access to services and making referrals. These referrals can become subject area to a lengthy filibuster, which may so result in demotivation. Furthermore, the participants felt advice between do nurses and community-based services impacted on diabetes management due to communication barriers and conflicting information, but they did not offer suggestions on how this situation could be improved.
Additional resource that were discussed were online services and health apps. Withal, while all the participants mentioned signposting patients to online resources, such as Diabetes UK, none discussed the value of such services, or whether they actively demonstrated this resource to the patients. In improver, limited attending was granted to the utilize of health apps. One of the possible reasons for this is alluded to below:
"That's the style we are all being pushed to go, but I'k really struggling getting people to engage… information technology's amazing just how many people only don't want information technology, not interested. Information technology's very time-consuming for us too but I do try, I do endeavour… you lot've got people there with smartphones sitting at that place in front end of you – I oasis't got an answer as to why they are not interested, because if you show them they announced interested but they don't – I can't think of one person that use the health app." Participant seven
This acknowledges that the employ of technology in self-management is pertinent but that there can be challenges in engaging people in its apply. Impediments to the employment of technology are, therefore, non simply structural (east.g. limited external capacity of services) only could also be a consequence of patient disposition, or nurse–patient interactions. As the participant highlighted, this is noteworthy considering the familiarity of smartphone usage for many people. Alternatively, information technology could exist that patients do non view the direction of their condition and personal resources such equally their phone as compatible. It is possible that a lack of compliance could impact upon nurse motivation (Jansink et al, 2010), leading them to feel less inclined to promote these resource. Further investigation is required to grasp why at that place could exist impediments to embedding technology within self-management.
Theme 3: Medication and prescribing
Medication was a further central theme raised across the interviews. This topic was salient for participants regardless of whether or not they were a qualified prescriber. Of the participants, the majority (v) were not in a prescribing role, and all of these had mixed perceptions on where their roles stood in terms of providing patients with medications. For example, Participant iv felt able to discuss alterations to medication with a GP, yet this would non involve the GP assessing the patient themselves. The heavy interest in the titration of medication was also conveyed by Participant 8:
"I do notice myself advising them on titration, which I suppose I shouldn't every bit I'm non a prescriber, simply what are you lot supposed to do? You can't just let the patients continue poorly controlled, and what a waste product of resource… if y'all referred anybody and then they accept to await ages." Participant eight
Partaking in this procedure is known as prescribing by proxy, significant nurses are independent in their decision-making regarding care and treatment, but accept no actual legal right to prescribe (Bradley et al, 2005).
Although only iii interviewees were qualified prescribers, their consistent view was that prescribing made their chore part easier and enhanced the quality of care. The following quote demonstrates this perspective, addressing how much the prescribing office assists:
"Massively because I can up and down prescriptions and alter things and information technology lets you do it holistically, and it saves the waiting time and talking to doctors, who perhaps don't always sympathize it as much as you do. They are just saying: 'what do yous desire to prescribe?'"Participant 7
However, another participant expressed unease with some of the updates available for prescribers on diabetes medication. They felt it was too complex and aimed at GPs, who ultimately practise not provide the reviews for patients:
"There are some updates available because we went to one last week with a drug rep. It was a scrap over my head, information technology was a bit as well – erm, what'south the word I'm looking for, erm – 'scientific'." Participant five
This could discourage prescribers from making the option to prescribe for patients with type 2 diabetes, potentially hindering the support of self-management. This is in line with the findings of Drennan et al (2014), who institute decreasing numbers of actively prescribing nurses within the Britain.
Study limitations
The limitations of the research design must be recognised. As a pocket-size-scale qualitative study with a focused sample, no claims to generalisability are made. The report relates to the detail experiences of a group of professionals inside ane region of the Britain.
Conclusions
Facilitating the self-management of type ii diabetes is a circuitous claiming, due to the latitude of factors that shape people's feel. Advice is cardinal to nurses' endeavours to facilitate effective self-management of the condition. Information technology is vital that communication is predicated on a sound understanding of each patient's disposition and circumstances, so that person-centred support tin exist delivered.
The patient–nurse interaction within main care, in itself, is not sufficient to ensure that high-level support of people with blazon 2 diabetes is achieved; a wider context of support also needs to be accessible. Increasing resource constraints upon health and social care services could therefore pose a challenge for practice nurses. The inclusion of the prescribing role within the practice nurse remit also shows how professional boundaries are constantly shifting. If role boundaries are unclear and access to external support is constrained, and so this could impede nurse–patient interactions where the goal is to facilitate the self-management of people with blazon two diabetes.
It is therefore recommended that greater attending should exist granted to ensuring clarity of part boundaries and also the nature of the relationship betwixt diabetes support and other services. This tin aid to generate a more coherent context within which the self-management of type 2 diabetes tin exist facilitated. Person-centred advice must also be reconciled with goal setting for patients, ensuring that goals are tangible, realistic and sustainable.
Source: https://diabetesonthenet.com/journal-diabetes-nursing/nurses-perspectives-supporting-self-management-type-2-diabetes-within-primary-care-setting/
0 Response to "Effective Nurse Communication With Type 2 Diabetes Patients a Review"
Post a Comment